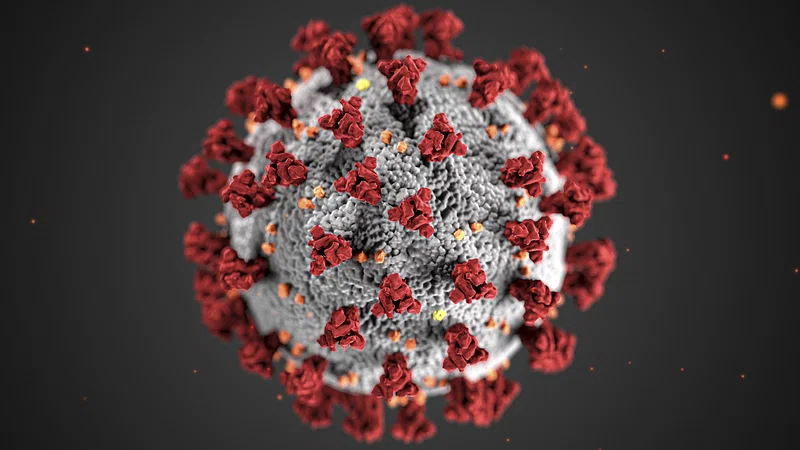
Though the public focus on COVID has waned, the virus continues to influence health care systems across the country. In 2025, COVID is considered endemic, with seasonal surges and new variants still under observation. A recent global report from the World Health Organization shows that test positivity rates have reached 11%, a figure comparable to levels seen during earlier summer waves. Emerging subvariants such as NB.1.8.1, sometimes referred to as “Nimbus,” are being monitored for changes in transmissibility. While vaccines and previous exposure reduce the likelihood of severe illness for many people, cases still rise in localized waves, prompting responses at the state and municipal level.
Ongoing Pressure on Hospitals and Clinics
COVID-related admissions have not returned to zero. The CDC continues to report hospitalizations connected to complications from the virus, particularly in patients over 65 or those with chronic illnesses. In some regions, early 2025 saw renewed mask advisories in clinics and emergency departments. Hospitals in cities like New York and St. Louis temporarily reinstated protective protocols after surges in respiratory illness. Although systems are better prepared than they were in 2020, each wave stretches resources—placing added stress on triage, staffing, and patient throughput.
Health Care Staffing and Burnout
The health care workforce has yet to fully recover from pandemic-era strain. While hiring across most hospital systems has rebounded, long-term effects persist in behavioral health, skilled nursing, and rural care. A University of Michigan report highlighted that staffing in these areas remains uneven, contributing to closures and service reductions. Rural hospitals, in particular, cite the compounded pressures of pandemic response and financial instability as leading causes of continued shutdowns in 2025. These losses further restrict access to in-person care and limit specialty coverage outside of urban centers.
Permanent Role of Telehealth Services
One of the most lasting effects of COVID on care delivery is the widespread adoption of telehealth. Virtual appointments became necessary during periods of isolation and lockdown, and they remain a standard offering in nearly every medical discipline. Telehealth supports patients in remote areas, increases access to mental health services, and reduces physical strain on high-volume hospitals. Providers have expanded the use of digital tools to monitor chronic disease, prescribe medications, and deliver follow-up care. This shift has helped ease congestion in outpatient clinics and emergency departments, especially during periods of increased viral transmission.
Health care systems now prioritize readiness in ways that were less common before 2020. Investments in surveillance, flexible infrastructure, and interdepartmental coordination have changed how health care organizations prepare for spikes in demand. The experience of the early pandemic led many institutions to reevaluate their approaches to supply management, respiratory illness protocols, and community engagement.
Mental Health Impacts on the Health Care Workforce
Provider mental health remains a pressing concern. Surveys continue to show high levels of burnout, anxiety, and stress among clinicians, especially nurses and emergency staff. Many professionals report that workloads have increased without a matching rise in support. Pandemic fatigue, combined with staffing gaps and rising patient needs, has left little room for recovery. Hospitals are now integrating mental health support programs, flexible scheduling, and peer support networks in an effort to maintain provider well-being and reduce turnover.
Continued COVID Vulnerability in High-Risk Groups
COVID continues to present risk for certain groups, particularly older adults, people with weakened immune systems, and those living in congregate care settings. For these populations, even moderate community spread can lead to serious complications. Infections may increase demand for respiratory therapy, intravenous hydration, or hospital admission. Providers caring for high-risk groups continue to prioritize vaccination, masking, and air filtration in shared settings. Many long-term care facilities operate with layered protections to reduce the likelihood of outbreaks, even during low transmission periods.